What is a TURP?
TURP stands for TransUrethral Resection of the Prostate. It is an operation that involves the removal of prostate tissue through an operating telescope (the resectoscope).
Who might need a TURP?
As the prostate is the gland that sits immediately below the bladder through which the urethra (the tube you pass your urine through) passes, it can block the flow of urine as it grows – as it does in all men. When this happens men usually notice they pass urine more slowly, go to the toilet more frequently and need to pass urine at night more often than usual. This can progress all the way to urinary retention – where a man cannot pass urine at all.
Men who have a TURP usually fall into one of the following categories and have:
-
Urinary retention.
-
Failed medical therapy.
-
Recurrent urinary tract infections.
-
Recurrent bleeding.
Are there alternatives?
There are a number of options available to treat symptoms caused by an enlarged prostate, though obviously not all are suitable for all men. Alternatives include:
-
Observation and monitoring.
-
Medical therapy.
-
Urolift device.
-
Laser prostatectomy (the same operation as a TURP using a laser as the tool to remove the tissue).
-
Open prostatectomy – very rarely advised as newer techniques can usually avoid the need for this old operation.
-
Long term catheterization – either urethral (through the penis) or suprapubic (through the lower abdomen).
How is a TURP performed?
The operation is performed under general or local (spinal) anaesthesia. The anaesthetist will discuss which is the best option for you – sometimes it is both.
The urethra, prostate and bladder are usually inspected at the commencement of the procedure to ensure there are no other abnormalities present. This is done utiising a cystoscope – a type of telescope.
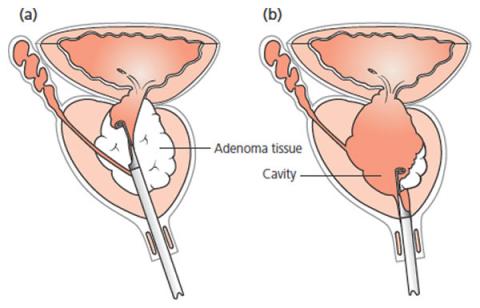
After this has been done a larger telescope (the resectoscope) is passed into the bladder and positioned at the level of the prostate. Depending on the exact equipment used a form of electrocautery is used to remove the obstructing prostate tissue, piece by piece. Once sufficient tissue has been removed, any bleeding is cauterized and any remaining pieces of prostate tissue removed from the bladder.
A 3-way indwelling catheter is then inserted into the bladder. This allows irrigation of fluid over the little while to make sure no clots can form in the bladder that might delay your recovery. It is usually removed 24-48 hours after the operation.
What happens after the operation?
The 3-way catheter will be irrigated, preventing any clot formation. There is usually little pain, though occasionally there is some bladder spasm that will be relieved with medication.
The catheter is removed 24-48 hours after the procedure. You will be discharged once you have successfully passed urine, and the nurse has determined you are not retaining excessive urine in your bladder.
For a few days after your procedure, it is normal to experience any of the following:
-
A mild burning when you pass your urine.
-
A need to pass urine more frequently, and occasionally more urgently than you usually do.
-
Some blood in the urine.
All usually settle quite rapidly without the need for any treatment.
What can you do to help?
-
Drink plenty of water.
-
Take Ural or Citravescent in a glass of water 4 times a day.
-
2 Panadol every 4 hours.
-
Take any antibiotics you have been prescribed.
Potential Side Effects
Most procedures are straightforward; however as with any surgical procedure there is a chance of side effects or complications.
Relatively Common
-
Mild burning, bleeding or frequency of urination after the procedure – this is only for a short time afterwards.
-
Retrograde ejaculation - no semen is produced during orgasm in 80% of men after a TURP. It does you no harm, though is an issue if you wish to have more children.
-
May not relieve all prostatic symptoms in approximately 5-10% of men.
Occasional
-
Erectile dysfunction – difficulty in achieving or maintaining an erection (5-10%). Some men find their sexual function improves after surgery.
-
Infection requiring antibiotics.
-
Finding unsuspected cancer in the removed prostate tissue or in the bladder, that may require further treatment.
-
Possible need to re-operate in future due to recurrent obstruction (10% over 10years).
-
Failure to pass urine after surgery requiring another catheter.
Rare
-
Bleeding requiring return to theatre and / or blood transfusion.
-
The need to self-catheterise after the procedure to fully empty the bladder.
-
Injury to urethra causing stricture – a scar in the urethra.
-
Temporary loss of urinary control (incontinence) – risk <0.5% long term.
-
Absorption of irrigation fluids causing confusion.
-
Very rarely perforation of the bladder requiring temporary insertion of a catheter or open surgical repair.
